子痫前期(pre-eclampsia,PE)是妊娠期特有的高血压性疾病,患者妊娠>20周出现蛋白尿、高血压、下肢水肿是其典型临床特征,若治疗不及时,可造成孕妇多器官系统的损伤,其中最常见的是肾损伤[1-2]。肾功能不全是孕妇发生不良妊娠结局(如流产、死胎、早产等)的危险因素,也是影响围产儿生命安全的主要原因[3]。PE肾损伤在早期是可逆的,但目前临床对肾损伤诊断不足,因此寻找一种敏感的、可靠的血清标志物来评估患者的早期肾损伤,对减轻肾功能损伤、改善预后具有重要意义。中性粒细胞/淋巴细胞比值(neutrophil to lymphocyte ratio,NLR)与高血压、肾损伤均具有一定的相关性,可能是通过高血压引起机体慢性炎症反应而引发肾损伤[4];血小板/淋巴细胞比值(platelet to lymphocyte ratio,PLR)是近期在肾脏疾病中研究较多的炎症标志物[5]。NLR、PLR水平与早期肾损伤的相关研究文献尚不多见。本研究旨在探讨NLR、PLR与PE患者早期肾损伤的关系,以期为临床应用提供理论依据。
1 资料与方法 1.1 一般资料选取2020年1月至2022年2月在本院产科接收的PE患者98例(PE组)、113例妊娠期高血压(gestational hypertension,GH)患者(GH组)。纳入标准:符合《妇产科学(第9版)》有关PE的诊断标准[6],且符合《妊娠期高血压疾病诊治指南(2020)》中关于妊娠期高血压的诊断标准[7];孕周>28周;单胎妊娠。排除标准:伴有肿瘤、自身免疫疾病、炎症性疾病、糖尿病、高血压、心脏疾病者;既往有反复流产和多次胎停育史以及合并甲状腺功能异常者。另选取同时期的健康孕妇作为对照组,排除妊娠期合并高血压、心脏疾病及早产、异位妊娠、流产等合并症。本研究所有孕妇知情、同意并签署知情同意书,且该研究于2021年3月获得本院伦理委员会的审批。
1.2 方法 1.2.1 实验室检测于入院当天采集外周空腹肘静脉血15 mL,采用日本SYSMEX全自动血液分析仪(型号:XE-2100)及配套设备检测中性粒细胞、淋巴细胞、血小板,并计算NLR、PLR。NLR=中性粒细胞计数/淋巴细胞计数,PLR=血小板计数/淋巴细胞计数;采用全自动生化分析仪(购自美国GE公司)检测尿素氮(urea nitrogen,BUN)、血肌酐(serum creatinine,Scr)、胱抑素C(cystatin C,Cys-C),计算预估肾小球滤过率(estimate glomerular filtration rate,eGFR);并于入院当天收集患者的24 h尿液,采用双缩脲法测定24 h尿蛋白定量。
1.2.2 PE患者早期肾损伤评估入院时依据PE患者无症状性蛋白尿和(或)血尿等临床症状来评估肾损伤情况。早期肾损伤患者一般无任何临床症状,少数患者可出现眼睑水肿,多数患者需通过尿检等常规检查(尿液、B超、肾功能检查等)发现尿液中存在蛋白尿或血尿。根据入院时PE患者是否发生肾损伤,将其分为未发生肾损伤组56例和已发生肾损伤组42例,比较2组的临床资料[包括既往PE史、既往肾病史、既往高血压史、前置胎盘、胎盘早剥、HELLP综合征、重度PE(收缩压在160 mmHg以上或舒张压在110 mmHg以上,并伴有血小板减少或肝肾功能异常等)、年龄、体质量指数(body mass index, BMI)、舒张压、收缩压]及实验室指标(包括NLR、PLR、BUN、Scr、Cys-C、24 h尿蛋白、eGFR)。
1.3 统计学分析采用SPSS 25.0软件行数据处理。符合正态分布的计量资料以x±s表示,2组间比较采用LSD-t检验,不符合正态分布的计量资料用M(P25,P75)表示,组间比较采用Kruskal Wallis H检验。计数资料以[n(%)]表示,组间对比进行χ2检验,3组间行F检验,采用Pearson相关系数进行相关性分析,通过多因素Logistic回归分析影响PE患者发生早期肾损伤的危险因素,根据受试者工作特征曲线分析法计算NLR、PLR诊断早期肾损伤的曲线下面积、敏感度、特异度。P < 0.05表示差异有统计学意义。
2 结果 2.1 3组研究对象一般资料、NLR、PLR水平及肾功能指标比较3组研究对象的年龄、BMI、孕周等一般资料差异无统计学意义,但GH组与PE组的NLR、BUN、Scr、Cys-C、24 h尿蛋白水平高于对照组,且PE组高于GH组(P < 0.05);PLR、eGFR水平低于对照组,且PE组低于GH组(P < 0.05),见表 1。
| 组别 | n | 年龄/岁 | BMI/(kg/m2) | 孕周/周 | NLR | PLR |
| 对照组 | 98 | 32(30,34) | 22.90±1.29 | 32.36±2.19 | 1.56±0.50 | 168.25±18.33 |
| GH组 | 113 | 33(31,34) | 23.03±1.32 | 32.41±2.22 | 2.43±0.68 | 121.36±17.35 |
| PE组 | 68 | 34(32,36) | 23.15±1.39 | 32.46±2.23 | 4.28±0.96 | 83.31±15.19 |
| H/F | 0.683 | 0.499 | 0.365 | 6.991 | 24.392 | |
| P | 0.514 | 0.835 | 0.922 | < 0.001 | < 0.001 | |
| 组别 | n | BUN/(mmol/L) | Scr/(μmol/L) | Cys-C/(mg/L) | 24 h尿蛋白/(g/24 h) | eGFR/[mL/(min·1.73 m2)] |
| 对照组 | 98 | 3.70±0.93 | 73.24±12.87 | 0.79±0.08 | 0.25±0.06 | 128.64±7.48 |
| GH组 | 113 | 4.92±0.96 | 96.38±15.08 | 2.33±0.75 | 3.27±1.01 | 99.28±6.53 |
| PE组 | 68 | 7.14±1.14 | 112.31±27.19 | 4.69±1.17 | 6.14±1.69 | 72.38±5.12 |
| F | 23.103 | 8.609 | 21.537 | 22.547 | 44.183 | |
| P | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |
2.2 NLR、PLR与肾功能指标的关系
经Pearson相关性分析可知,NLR与BUN、Scr、Cys-C、24 h尿蛋白呈正相关(r=0.592,P < 0.001;r= 0.517,P < 0.001;r=0.489,P < 0.001;r=5.785,P < 0.001),与eGFR呈负相关(r=-0.513,P < 0.001);PLR与BUN、Scr、Cys-C、24 h尿蛋白呈负相关(r=-6.384,P < 0.001;r=-5.588,P < 0.001;r=-4.439,P < 0.001;r= 5.491,P < 0.001),与eGFR呈正相关(r=0.582,P < 0.001)。
2.3 PE患者发生早期肾损伤的影响因素98例PE患者中发生早期肾损伤42例,占比42.86%。单因素分析显示,既往PE史、既往肾病史、HELLP综合征、重度PE、年龄、血压、NLR、PLR、BUN、Scr、Cys-C、24 h尿蛋白、eGFR是PE患者发生早期肾损伤的影响因素(P < 0.05,表 2);多因素分析显示,重度PE、NLR、PLR、24 h尿蛋白、eGFR是影响PE患者发生早期肾损伤的主要危险因素(P < 0.05,表 3)。
| 组别 | n | 既往PE史 | 既往肾病史 | 既往高血压史 | 前置胎盘 | 胎盘早剥 | HELLP综合征 |
| 未发生肾损伤组 | 56 | 0 | 2(3.57) | 8(14.29) | 5(8.93) | 6(10.71) | 3(5.36) |
| 已发生肾损伤组 | 42 | 5(11.90) | 7(16.67) | 8(19.05) | 5(11.90) | 7(16.67) | 9(21.43) |
| χ2 | 7.025 | 4.579 | 0.398 | 0.232 | 0.739 | 5.769 | |
| P | < 0.001 | < 0.001 | >0.05 | >0.05 | >0.05 | < 0.001 | |
| 组别 | n | 重度PE | 年龄/岁 | BMI/(kg/m2) | 舒张压/(mmHg) | 收缩压/(mmHg) | NLR |
| 未发生肾损伤组 | 56 | 14(25.00) | 28.46±3.84 | 23.15±2.04 | 95.36±3.18 | 140.62±5.06 | 2.69±0.75 |
| 已发生肾损伤组 | 42 | 22(52.38) | 43.59±5.38 | 23.20±2.13 | 119.37±6.03 | 163.28±9.21 | 4.83±1.24 |
| χ2/t | 7.742 | 16.023 | 0.119 | 25.473 | 15.561 | 10.594 | |
| P | < 0.001 | < 0.001 | >0.05 | < 0.001 | < 0.001 | < 0.001 | |
| 组别 | n | PLR | BUN/(mmol/L) | Scr/(μmol/L) | Cys-C/(mg/L) | 24 h尿蛋白/(g/24 h) | eGFR/[mL/(min·1.73m2)] |
| 未发生肾损伤组 | 56 | 118.45±17.69 | 5.09±1.03 | 98.02±15.11 | 2.39±0.80 | 3.36±1.37 | 98.54±6.63 |
| 已发生肾损伤组 | 42 | 80.94±15.02 | 7.28±1.23 | 114.65±26.30 | 4.85±1.28 | 6.22±1.82 | 70.60±5.34 |
| t | 11.068 | 9.581 | 3.946 | 11.670 | 6.879 | 22.393 | |
| P | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |
| 指标 | β | SE | Wald χ2 | P | OR | 95%CI |
| 重度PE | 0.743 | 0.629 | 11.527 | 0.002 | 2.109 | 2.064~2.889 |
| NLR | 0.844 | 0.380 | 11.663 | < 0.001 | 2.302 | 2.101~2.998 |
| PLR | 0.872 | 0.220 | 18.334 | 0.001 | 2.476 | 2.165~2.999 |
| 24 h尿蛋白 | 0.458 | 0.426 | 5.097 | 0.028 | 1.560 | 1.120~1.974 |
| eGFR | 0.746 | 0.536 | 9.810 | 0.007 | 1.638 | 1.073~2.006 |
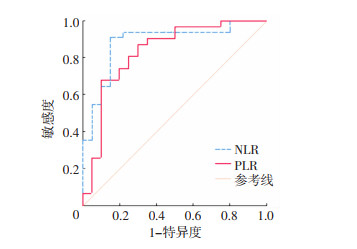
2.4 NLR、PLR对PE患者发生早期肾损伤的预测价值
受试者工作特征曲线分析发现,NLR、PLR预测PE患者发生早期肾损伤的截断值分别为2.71、103.26,曲线下面积分别为0.896、0.809,敏感度分别为93.28%、90.81%,特异度分别为80.17%、80.01%, 见表 4、图 1。
| 指标 | 截断值 | 曲线下面积 | 95%CI | 敏感度/% | 特异度/% | P |
| NLR | 2.71 | 0.896 | 0.786~0.983 | 93.28 | 80.17 | < 0.001 |
| PLR | 103.26 | 0.809 | 0.658~0.961 | 90.81 | 80.01 | < 0.001 |
|
| 图 1 NLR、PLR预测PE患者早期肾损伤的受试者工作特征曲线 |
3 讨论
肾损伤是子痫前期最常见、最严重的并发症,可导致肾脏发生一系列的病理性损伤,严重者甚至会造成不可逆损伤,如肾衰竭、肾皮质坏死等[8]。本研究结果表明,98例PE患者中有56例发生早期肾损伤,发生率为57.14%,提示PE患者的肾损伤发生率较高。因此早期有效评估PE患者肾损伤对改善预后、制订合理治疗方案至关重要。
BUN、Scr、Cys-C、24 h尿蛋白、eGFR是反映肾功能的传统指标,有研究显示,Cys-C对肾脏疾病的早诊断、早治疗具有指导意义[9-10];24 h尿蛋白定量对肾脏疾病治疗的指导、疗效的评价、预后的判断均具有重要的作用[11-12];eGFR对肾脏疾病的诊断、治疗方案的确定也具有一定的指导意义[13]。但有研究证实,24 h尿蛋白、eGFR预测PE患者早期肾损伤的敏感度不高,对患者早期肾损伤的预后评估也具有一定的局限性[14]。PE患者发生肾损伤的主要机制是:子痫前期母体对妊娠是一种过度的炎症反应,再加上母体持续高血压引发的慢性炎症反应引发全身小血管痉挛,致血压升高,全身各脏器血容量减少,进而加重肾脏组织及细胞的损伤,而NLR、PLR与炎症反应相关,已有文献表明,NLR、PLR参与了PE的发生、发展及预后[15-16]。本研究结果发现,已发生肾损伤组NLR、PLR、Cys-C、24 h尿蛋白较未发生肾损伤组更高,eGFR较未发生肾损伤组更低,说明PE患者早期肾损伤NLR、PLR显著升高,推测NLR、PLR可能与PE患者肾损伤相关。
本研究结果显示,重度PE、NLR、PLR、24 h尿蛋白、eGFR是PE患者早期肾损伤的独立危险因素,且NLR、PLR预测PE患者早期肾损伤的曲线下面积分别为0.896、0.809,敏感度分别为93.28%、90.81%,特异度分别为80.17%、80.01%,充分说明NLR、PLR与PE患者早期肾损伤有关,且预测价值较高。有研究表明,NLR、PLR作为非特异性系统炎症指标参与了多种肾脏疾病的发生、发展过程[17-18]。NLR是中性粒细胞(炎症激活因子)与淋巴细胞(炎症调节因子)的比值,NLR水平越高表示机体内的炎症状态越严重,可有效反映心血管患者的炎症反应状态[19]。PLR是血小板与淋巴细胞的比值,血小板可以与内皮细胞、T淋巴细胞等多种不同细胞相互作用,启动并加剧炎症反应,导致肾脏组织及细胞程度加重,患者预后不佳[7]。NLR可影响肾脏疾病患者炎症反应的发生、发展、预后,一项包含4 997例患者的Meta分析证实,NLR可引发并进一步加重急性肾损伤,可作为急性肾损伤的重要预测工具[20]。王小娟等[21]在280例重症合并急性肾损伤的患者中发现,PLR可加剧炎症反应,并进一步增加肾脏组织、细胞的受损程度。因此,当PE患者体内的PLR呈高表达时,可明显增加早期肾损伤发生的风险。
综上所述,NLR、PLR水平升高与PE患者早期肾功能损伤有关,且二者在临床实际工作中很容易获得;同时,多项研究均以证实NLR、PLR在PE及相关并发症(如肾损伤)的预测中发挥着至关重要的作用[22-23],能够帮助临床医师简单获取并早期识别PE早期肾损伤的发生。NLR、PLR也是PE患者早期肾损伤的独立危险因素,对早期肾损伤有较高的预测价值。但本研究样本量较小,仍需进一步完善随机、多中心的试验进行验证与研究。
| [1] |
刘丹, 苟文丽, 李雪兰, 等. 血清PODXL监测子痫前期早期肾脏损伤的初步研究[J]. 现代妇产科进展, 2020, 29(9): 668-671. LIU D, GOU W L, LI X L, et al. Primary study of serum PODXL in monitoring early renal injury in preeclampsia[J]. Prog Obstet Gynecol, 2020, 29(9): 668-671. |
| [2] |
毛艳, 赵茵. 子痫前期肾损伤的研究进展[J]. 中国实用妇科与产科杂志, 2022, 38(1): 113-116. MAO Y, ZHAO Y. Research progress of renal injury in preeclampsia[J]. Chin J Pract Gynecol Obstet, 2022, 38(1): 113-116. |
| [3] |
王永萍, 王莉. 妊娠期高血压疾病的危险因素和母儿结局分析[J]. 中国临床医生杂志, 2022, 50(5): 600-602. WANG Y P, WANG L. Analysis of risk factors and maternal and fetal outcomes of hypertensive disorder complicating pregnancy[J]. Chin J Clin, 2022, 50(5): 600-602. |
| [4] |
张瑶, 杨心宇, 陈洲芳. 神经突起导向因子1和中性粒细胞/淋巴细胞与妊娠期高血压疾病早期肾损伤的相关性[J]. 中华高血压杂志, 2019, 27(10): 971-974. ZHANG Y, YANG X Y, CHEN Z F. Correlation between neurite guiding factor 1 and neutrophils/lymphocytes and early renal injury in hypertensive disorder complicating pregnancy[J]. China J Hypertens, 2019, 27(10): 971-974. |
| [5] |
何家燕, 廖琳, 唐金城, 等. 血小板/淋巴细胞比值、中性粒细胞/淋巴细胞比值与慢性肾脏病关系的研究进展[J]. 临床肾脏病杂志, 2019, 19(3): 214-218. HE J Y, LIAO L, TANG J C, et al. Research advances in relationship of neutrophil/lymphocyte ratio and platelet/lymphocyte ratio with chronic kidney diseases[J]. J Clin Nephrol, 2019, 19(3): 214-218. |
| [6] |
谢幸, 孔北华, 段涛. 妇产科学[M]. 9版. 北京: 人民卫生出版社, 2018: 83. XIE X, KONG B H, DUAN T. Obstetrics and gynecology[M]. 9th. Beijing: People's Medical Publishing House, 2018: 83. |
| [7] |
中华医学会妇产科学分会妊娠期高血压疾病学组. 妊娠期高血压疾病诊治指南[J]. 中华妇产科杂志, 2020, 55(4): 227-238. Pregnancy-induced Hypertension Disease Group of Obstetrics and Gynecology Branch of Chinese Medical Association. Diagnosis and treatment of hypertension and pre-eclampsia in pregnancy: a clinical practice guideline in China(2020)[J]. Chin J Obstet Gynecol, 2020, 55(4): 227-238. |
| [8] |
郭雪晶, 黄鹰, 张羽. Sema3A、KIM-1和Cys C在子痫前期患者肾功能损害早期诊断中的临床价值[J]. 河北医科大学学报, 2019, 40(11): 1285-1289. GUO X J, HUANG Y, ZHANG Y. Clinical value of Sema 3A, KIM-1 and Cys C in the early diagnosis of renal impairmentin pre-eclampsia[J]. J Hebei Med Univ, 2019, 40(11): 1285-1289. |
| [9] |
王肇. 血清sEng、sFlt-1和Cys C在妊娠期高血压疾病肾功能损害中的临床诊断价值[J]. 检验医学与临床, 2022, 19(S02): 60-64. WANG Z. Clinical diagnostic value of serum sEng, sFlt-1 and Cys C in renal dysfunction in hypertensive disorders complicating pregnancy[J]. Lab Med Clin, 2022, 19(S02): 60-64. |
| [10] |
GOMES H C D S, CABRAL A C V, ANDRADE S P, et al. Cystatin C as an indicator of renal damage in pre-eclampsia[J]. Hypertens Pregnancy, 2020, 39(3): 308-313. |
| [11] |
刘杰, 陈静静. 尿蛋白定量检测在糖尿病肾损害诊断中的临床意义[J]. 标记免疫分析与临床, 2020, 27(1): 86-89. LIU J, CHEN J J. The clinical significance of quantitative detection of urinary protein in the diagnosis of diabetic renal damage[J]. Lab Immun Clin Med, 2020, 27(1): 86-89. |
| [12] |
HERMAN H G, BARDA G, MIREMBERG H, et al. Management of pregnancies with suspected preeclampsia based on 6-hour vs 24-hour urine protein collection—a randomized double-blind controlled pilot trial[J]. Am J Obstet Gynecol MFM, 2021, 3(5): 100429. |
| [13] |
FIACCO F, MELANDRO F, UMBRO I, et al. Fluctuations of estimated glomerular filtration rate outside kidney disease improving global outcomes diagnostic criteria for acute kidney injury in end-stage liver disease outpatients and outcome postliver transplantation[J]. Transplant Direct, 2018, 4(1): e222. |
| [14] |
LI Y T, LIU C H, WANG P H. Serum cystatin C or cystatin C-based glomerular filtration rate may be a better choice in estimating renal function in women with preeclampsia[J]. Taiwan J Obstet Gynecol, 2021, 60(5): 801-802. |
| [15] |
喻红彪, 史梦丹, 姚静, 等. 孕期中性粒细胞/淋巴细胞比值与血小板/淋巴细胞比值预测子痫前期的价值[J]. 四川大学学报(医学版), 2022, 53(6): 1039-1044. YU H B, SHI M D, YAO J, et al. Value of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio for predicting preeclampsia during pregnancy[J]. J Sichuan Univ Med Sci, 2022, 53(6): 1039-1044. |
| [16] |
龙黎南, 黄鹰, 张治萍, 等. 中性粒细胞/淋巴细胞比值和血小板/淋巴细胞比值与子痫前期严重程度的相关性[J]. 中国妇幼保健, 2021, 36(6): 1263-1266. LONG L N, HUANG Y, ZHANG Z P, et al. Correlation between neutrophil/lymphocyte ratio and platelet/lymphocyte ratio and severity of preeclampsia[J]. Matern Child Health Care China, 2021, 36(6): 1263-1266. |
| [17] |
吴苏, 戴雅丽, 王阳阳, 等. 中性粒细胞/淋巴细胞比值和血小板/淋巴细胞比值与2型糖尿病患者肾小管损伤的相关性研究[J]. 中华糖尿病杂志, 2021, 13(1): 66-72. WU S, DAI Y L, WANG Y Y, et al. Association between neutrophil-to-lymphocyte or platelet-to-lymphocyte and renal tubular injury in type 2 diabetes mellitus patients[J]. Chin J Diabetes Mellit, 2021, 13(1): 66-72. |
| [18] |
MAE Y, TAKATA T, IDA A, et al. Prognostic value of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio for renal outcomes in patients with rapidly progressive glomerulonephritis[J]. J Clin Med, 2020, 9(4): 1128. |
| [19] |
CHEN Z N, HUANG Y R, CHEN X, et al. Value of neutrophil-to-lymphocyte ratio as a marker of renal damage in patients with H-type hypertension[J]. Biomark Med, 2021, 15(9): 637-646. |
| [20] |
卢志, 王立华, 贾岚, 等. 中性粒细胞与淋巴细胞比值对急性肾损伤预测作用的Meta分析[J]. 中华危重病急救医学, 2021, 33(3): 311-317. LU Z, WANG L H, JIA L, et al. A meta-analysis of the predictive effect of neutrophil-lymphocyte ratio on acute kidney injury[J]. Chin Crit Care Med, 2021, 33(3): 311-317. |
| [21] |
王小娟, 陆士奇, 徐进步, 等. 血小板与淋巴细胞比值在重症患者合并急性肾损伤中的临床应用价值[J]. 中国急救医学, 2019, 39(8): 763-766. WANG X J, LU S Q, XU J B, et al. Clinical study of platelet-to-lymphocyte ratio among critically ill patients with acute kidney injury[J]. Chin J Crit Care Med, 2019, 39(8): 763-766. |
| [22] |
张瑶, 杨心宇, 陈洲芳. 神经突起导向因子1和中性粒细胞/淋巴细胞与妊娠期高血压疾病早期肾损伤的相关性[J]. 中华高血压杂志, 2019, 27(10): 971-974. ZHANG Y, YANG X Y, CHEN Z F. Correlation between neurite guiding factor 1 and neutrophils/lymphocytes and early renal injury in hypertensive disorder complicating pregnancy[J]. Chin J Hypertens, 2019, 27(10): 971-974. |
| [23] |
Mae Y, Takata T, Ida A, et al. Prognostic value of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio for renal outcomes in patients with rapidly progressive glomerulonephritis[J]. J Clin Med, 2020, 9(4): 1128. |




