传统观点认为,膝关节置换(total knee arthroplasty, TKA)时恢复下肢中立位力线(neutral mechanical axis)可使内外侧平台均匀负重,降低假体磨损及松动,相反,下肢力线恢复不充分则会影响假体的生存率,为避免中远期置换失败,(0±3)°的下肢力线通常被认为是可以接受的[1-5]。然而,术后患者不满意度仍高达20%~25%[6]。BELLEMANS等[7]的研究指出大部分正常人的下肢力线并不是中立位,而是存在≥3°的内翻,男性、女性占比分别为32%和17%,自骨骼发育成熟以来这部分人群下肢力线就处于内翻状态,已适应该内翻力线。如果在TKA时采用韧带松解、股骨或胫骨截骨等技术过度矫正下肢力线至中立位,既不正常,还会导致术后膝关节的不自然。研究证实下肢力线内翻与股骨颈干角(femoral neck-shaft angle, NSA)减小、增加的冠状面股骨外弓(coronal femoral lateral bowing, CFLB)以及关节外畸形等有关[8-10]。还有研究指出,与完全恢复中立位相比,对术前下肢力线即存在内翻的患者,残留轻度内翻(>3°~6°)将具有更好的临床功能评分[11-17]。在亚洲地区,股骨冠状面外弓的发病率达到62%以上[18-19]。在日常临床工作中,我们也发现许多中国患者存在下肢股骨的冠状面外弓,导致术前下肢力线内翻。因此,本研究对股骨存在外弓及内侧膝骨关节炎(medial osteoarthritis of the knee, MOA)的TKA术后患者进行随访,将患者术后下肢力线按轻度(>3°~6°)、中度、重度内翻分为3组,了解轻度内翻是否影响股骨外弓MOA患者术后的功能结果。
1 资料与方法 1.1 一般资料本研究采用回顾性队列研究设计,对2015年1-12月在我科完成TKA手术的152例患者进行随访。比较各组间的KSS及WOMAC评分,了解轻度内翻是否影响股骨外弓MOA患者术后的功能结果。诊断标准:影像学检查提示以内侧间室退行性改变为主,符合Kellgren-Lawrence放射学诊断标准Ⅲ级及以上。纳入标准:①疼痛集中在膝关节内侧间室,髌股关节无明显症状,下肢力线内翻;②前交叉韧带及内侧副韧带功能正常;③患者心肺功能等能耐受手术、配合术后康复训练及按时随访;④术前C反应蛋白(C-reaction protein, CRP)、降钙素原(procalcitonin, PCT)、血沉(erythrocyte sedimentation rate, ESR)在正常范围;⑤术后1年内均未出现感染或肿瘤等情况。排除标准:感染性膝关节炎、创伤性关节炎、胫骨存在畸形、膝关节外翻畸形、既往曾行过股骨或胫骨的截骨矫形手术以及存在除股骨外弓以外原因导致的下肢力线内翻患者。本研究所有患者术前均签署知情同意书。
1.2 手术方式所有手术由同一个手术医师完成。麻醉生效后,患者取平卧位,术野常规碘伏、酒精消毒,铺无菌巾单。驱血,气囊止血带止血。取膝前正中切口,上起于髌骨上方腱腹交界处,止于胫骨结节内侧1 cm。切开皮肤、皮下组织,自股直肌与股内侧肌间隙腱腹交界处,向远端沿髌骨内侧切开肌腱、关节囊及髌内侧支持带。切除滑膜及髌下部分脂肪垫,于胫骨结节内侧1 cm处切开骨膜,沿骨膜下锐性剥离,初步松解内侧关节囊,将髌骨外翻,屈膝关节,咬骨钳咬除股骨及胫骨骨赘,切除增生滑膜、半月板及前、后交叉韧带。将胫骨平台向前脱位,清理残余滑膜、半月板、骨赘,注意保护内侧副韧带。安装胫骨髓外定位器,胫骨进针点位于髁间嵴前方、前交叉韧带止点中央、胫骨结节内1/3,与胫骨中心线相一致。安装截骨器,注意保持定位杆指向踝关节中心大约1、2趾之间,与胫骨力线平行,于胫骨近端安装胫骨截骨器。垂直胫骨力线沿内侧平台最低点定位截骨厚度,于刻度“0”处定位胫骨平台截骨板并后倾3°截骨,用摆锯切除胫骨平台关节面,修剪平台边缘,测试胫骨平台假体大小。从股骨髁间窝上方,后交叉韧带止点前5 mm置入股骨髓内杆,选取合适外翻角安放定位器。用定位器定位,安放股骨远端截骨器,取下髓内定位器,行股骨远端截骨,以间隙试模测伸直间隙,见膝关节可完全伸直,力线正常,侧向稳定。测股骨远端假体大小,以合适的外旋角度安放截骨器,分别行股骨前髁、后髁及两个斜面截骨。取下截骨器,以间隙试模测屈膝间隙,见间隙合适,与伸直间隙一致。安放股骨髁间截骨器,稍偏外侧行髁间截骨。于股骨侧、胫骨侧安放假体试模和衬垫,复位后见力线好,关节松紧适宜,屈伸膝关节,见屈伸间隙合适,取出试模冲洗切口,调好骨水泥,计时安放膝关节胫骨、股骨假体及衬垫。伸直位保持计时至骨水泥完全固化后行髌骨去神经化处理,切除髌骨边缘骨赘,修整关节面,测试髌骨运行轨迹良好。大量生理盐水冲洗伤口后复位膝关节,测力线经过髌骨正中,伸屈适宜。清点器械敷料无误,松开止血带止血后逐层缝合髌内侧关节囊、腱膜、皮下、皮肤,敷料覆盖切口,弹力绷带包扎。患者安返病房。人工全膝关节假体由Smith & Nephew公司提供。
1.3 术后处理术后所有患者统一康复治疗方案:麻醉复苏后即开始行踝泵训练,行股四头肌力量和膝关节主被动屈伸功能锻炼;第2天无特殊情况所有患者均下地扶助行器行走;术后常规预防血栓、感染,待患者膝关节主动完全伸直、屈曲超过120°时复查膝关节X片及标准的双下肢全长片,根据术后下肢力线(mechanical femorotibial alignment,FTMA)——股骨头中心(H)到膝关节中心(K)的连线与膝关节中心到踝关节中心(A)连线的夹角,将患者分为A、B、C 3组,分别为轻度内翻(>3°~6°,n=45),重度内翻(>6°,n=26)及中立位组[(0±3)°,n=81]。分别在术前及术后最后随访点时对患者进行国际膝关节协会(international knee society score, KSS)及西安大略和麦克马斯特大学骨关节炎指数(Western Ontario and McMaster University Osteoarthritis Index, WOMAC)评分。
1.4 术后随访术后对患者行KSS、WOMAC评分,并统计患者术后最后1次随访时的相关并发症,主要包括任何原因导致的翻修、无菌性松动、假体周围骨折、假体周围感染(periprosthetic joint infection,PJI)、深静脉血栓形成、麻醉下手法松解或手术松解等。
1.5 统计学分析对所有随访患者进行下肢力线测量,分析患者术后最后一次随访时的KSS、WOMAC评分,所有数据采用 x±s表示,符合正态分布的计量资料录入SPSS 19.0软件进行独立样本t检验,以P < 0.05为差异有统计学意义。
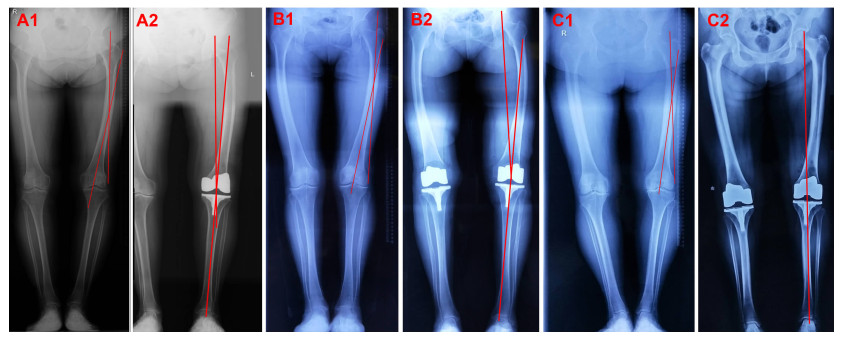
2 结果 2.1 患者基本资料及术前、术后下肢力线测量结果患者术前基本资料见表 1,所有患者存在下肢股骨的冠状面外弓。A组从术前的(9.8±3.2)°到术后的(4.3±0.6)°,B组从术前的(10.8±1.6)°到术后的(7.1±1.2)°,C组力线从术前的(8.8±3.5)°恢复到术后的(0.6±1.3)°,见图 1。
| 组别 | n | 年龄/岁 | BMI/kg·m-2 | 女性/男性 | 术前下肢力线/° |
| 中立位(C组) | 80 | 73.8±8.1 | 29.1±4.6 | 58/23 | 8.8±3.5 |
| 轻度内翻(A组) | 45 | 74.2±7.9 | 30.2±4.5 | 27/18 | 9.8±3.2 |
| 重度内翻(B组) | 26 | 77.5±7.3 | 31.2±5.5 | 14/12 | 10.8±1.6 |
|
| A1:轻度内翻组患者术前下肢全长片;A2:轻度内翻组显示术后平均下肢力线为偏离0°力线3°~6°;B1:重度内翻组患者术前下肢全长片;B1:重度内翻组显示术后平均下肢力线为偏离0°力线>6°;C1:中立位力线组患者术前下肢全长片;C2:中立位力线组显示术后下肢力线平均为偏离0°力线-3°~3° 图 1 合并股骨外弓的内侧膝骨关节炎患者术前下肢全长片及术后下肢力线测量 |
2.2 随访结果
随访3.1~5.2 (4.3±1.2)年,到随访终点为止,没有发现因机械性、无菌性松动或聚乙烯磨损造成的翻修患者,没有患者发生假体周围骨折、假体周围感染、深静脉血栓形成、麻醉下手法松解或手术松解等。
如表 2所示,C组、A组及B组术前KSS评分差异无统计学意义;TKA术后各组KSS评分均有所提高。与C组(P=0.02)及B组(P=0.01)相比,A组KSS评分提高更显著;在功能评分上获得了相近的研究结果,与C组及B组相比(P=0.01,P=0.04),A组KSS评分提高更显著;膝关节评分上,A组较B组改善更明显(P=0.03),但与C组相似。
| 组别 | n | 术前膝关节评分 | 术前功能评分 | 术前总KSS | 术后膝关节评分 | 术后功能评分 | 术后总KSS |
| 中立位(C组) | 81 | 62.0±12.1 | 52.0±21.2 | 114.0±24.2 | 87.0±12.7 | 70.0±15.2 b | 157.0±29.4b |
| 轻度内翻(A组) | 45 | 56.1±14 | 49.9±20.2 | 106.0±23.3 | 87.2±13.1a | 80.3±13.3a | 167.5±26.1a |
| 重度内翻(B组) | 26 | 60.8±13.2 | 47.4±23.1 | 108.2±28.9 | 79.8±11.2 | 71.1±12.2 | 150.9±32.3 |
| a:P < 0.05,与重度内翻组比较;b:P < 0.05,与轻度内翻组比较 | |||||||
如表 3所示,术后C组、A组及B组WOMAC疼痛评分差异无统计学意义;僵硬评分A组与C组(P=0.03)、A组与B组(P=0.04)之间差异具有统计学意义;日常活动度(activities of daily living, ADL)评分A组与C组(P=0.02)、A组与B组(P=0.04)之间差异有统计学意义;与C组及B组相比,A组具有更低的WOMAC评分(P=0.02,P=0.01);C组和B组具有相似的WOMAC评分。
| 组别 | n | 疼痛 | 僵硬 | 活动度 | 总体WOMAC评分 |
| 中立位(C组) | 81 | 4.3±4.6 | 2.5±2.0a | 20.1±18.2a | 25.3±24.1 a |
| 轻度内翻(A组) | 45 | 2.7±3.0 | 1.6±1.5b | 11.6±13.2b | 14.6±15.2b |
| 重度内翻(B组) | 26 | 4.5±4.0 | 2.8±1.8 | 24.7±20.5 | 24.9±20.7 |
| a:P < 0.05,与轻度内翻组比较;b:P < 0.05,与重度内翻组比较 | |||||
3 讨论 3.1 中立位力线及其对TKA的传统意义
下肢中立位力线被定义为一条从股骨头中心到距骨中心的直线。传统观点认为,TKA时需恢复下肢力线至中立位,即膝关节假体的中心位于股骨头中心与踝关节中心连线上,如此可使膝关节内外侧平台均匀负重,避免假体早期磨损及松动,大部分学者认为偏离下肢中立位(0±3)°的下肢力线是可以接受的[20-22]。然而,术后患者不满意度仍高达20%~25%[6]。
3.2 机械轴变异及股骨冠状面外弓BELLEMANS等[7]的研究指出,大部分正常人的下肢力线并不是中立位的,而是存在≥3°的内翻,男、女性占比分别为32%和17%。研究证实下肢力线内翻与股骨颈干角(femoral neck-shaft angle, NSA)减小、增加的冠状面股骨外弓(coronal femoral lateral bowing, CFLB)以及关节外畸形等有关[8-10]。CFLB在中国乃至亚洲人群中非常普遍。这部分患者自骨骼发育成熟以来下肢力线就处于内翻状态,已适应该内翻力线,如果在TKA时采用韧带松解、股骨或胫骨截骨等技术过度矫正下肢力线至中立位,事实上对患者自身而言既不正常,还会导致术后膝关节的不自然。
3.3 下肢内翻力线一定不好吗?PARRATTE等[24]对398例TKA患者进行15年的Kaplan-Meier生存率分析,发现中立位对线组和内翻对线组间差异并无统计学意义,为此研究指出:用“对位对线”良好和不良来预测TKA术后假体的生存时间是无用的。许多学者也提出了类似的建议[23, 25-27],对TKA术后患者进行下肢力线分析,并确定最严重的内翻对线不良患者,比较影像学、KSS及WOMAC评分、膝关节的活动范围等,他们指出:①导致TKA术后无菌性松动的原因很多,下肢力线可能并不是导致无菌性松动的最重要原因;②整体的下肢内翻力线与假体失败率的增加并无显著相关性;③与重建中立位力线组相比,残留轻度的下肢内翻力线可能会获得更好的临床和功能结果,轻度的内翻矫正不足并不会影响假体的长期生存率。本研究所有患者术前即存在股骨的冠状面外弓,即内翻的下肢力线,既往已有研究指出恢复患者术前的生理性内翻力线,膝关节周围的韧带张力将更接近术前的生理状态,TKA术后患者将具有更理想的临床及功能结果[28]。诚然,研究中所有组KSS评分均有所提高,但与中立位组(P=0.02)及重度内翻组(P=0.01)相比,轻度内翻组KSS评分提高更显著;在功能评分上也获得了相似的研究结果,与中立位及重度内翻组相比(P=0.01,P=0.04),轻度内翻组KSS评分提高更显著;膝关节评分上,轻度内翻组也较重度内翻组改善更明显(P=0.03),但与中立位组相似。VANLOMMEL等[29]对172例TKA患者(患者术前即存在下肢力线的内翻)进行5~9年的随访研究,结果显示术后下肢力线轻度内翻的患者不仅在临床和功能结果方面更优于重度内翻和中立位力线组,而且KSS和WOMAC评分改善也最大。SCHIFFNER等[30]也指出残留轻度的下肢内翻力线,对于术前即存在下肢内翻力线的患者将有更好的临床效果。
在本研究纳入随访研究的所有病例中,无论是术后力线偏离中立位超过6°,还是在-3°~3°范围内的中立位组,短期随访时间内均未发现有因机械性、无菌性松动或聚乙烯磨损造成的翻修患者,没有患者发生假体周围骨折、假体周围感染、深静脉血栓形成、麻醉下手法松解或手术松解等的患者。
与传统假体不同,本研究使用的是现代人工膝关节假体,改良的假体耐磨性能及设计参数对假体的生存率和术后功能评分有一定的改善。但PARATTEETAL等[23, 31-32]前期使用现代假体研究下肢力线与假体生存率之间的关系,并未发现假体安放在轻度内翻位或中立位之间存在统计学差异。
3.4 本研究的局限性首先,本研究随访时间较短,缺乏中长期研究结果,需要后期跟踪随访。其次,本研究只讨论了股骨外弓这一种下肢力线内翻患者,缺乏对因胫骨侧内翻畸形、韧带张力不平衡、骨缺损等原因所致内翻畸形病例的研究,需进一步对这类患者进行分析。
综上所述,虽然恢复中立位力线是一个成功膝关节置换的合理目标,但其证据并不确凿,存在争议,轻度内翻的下肢力线并不一定会导致更坏的效果,尤其对于术前即存在下肢内翻力线的患者。
| [1] |
LEE B S, LEE S J, KIM J M, et al. No impact of severe Varus deformity on clinical outcome after posterior stabilized total knee arthroplasty[J]. Knee Surg Sports Traumatol Arthrosc, 2011, 19(6): 960-966. |
| [2] |
MAGNUSSEN R A, WEPPE F, DEMEY G, et al. Residual Varus alignment does not compromise results of TKAs in patients with preoperative Varus[J]. Clin Orthop Relat Res, 2011, 469(12): 3443-3450. |
| [3] |
MATZIOLIS G, ADAM J, PERKA C. Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement[J]. Arch Orthop Trauma Surg, 2010, 130(12): 1487-1491. |
| [4] |
PARRATTE S, PAGNANO M W, TROUSDALE R T, et al. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements[J]. J Bone Joint Surg Am, 2010, 92(12): 2143-2149. |
| [5] |
王波, 胡海涛, 潘健, 等. 膝关节骨性关节炎全膝关节置换术后下肢力线与早期临床效果关系的研究[J]. 中国骨与关节损伤杂志, 2015, 30(10): 1044-1048. WANG B, HU H T, PAN J, et al. Relationship between lower limb alignment and early clinical results after TKA for osteoarthritis[J]. Chin J Bone Jo Inj, 2015, 30(10): 1044-1048. |
| [6] |
HOWELL S M, PAPADOPOULOS S, KUZNIK K T, et al. Accurate alignment and high function after kinematically aligned TKA performed with generic instruments[J]. Knee Surg Sports Traumatol Arthrosc, 2013, 21(10): 2271-2280. |
| [7] |
BELLEMANS J, COLYN W, VANDENNEUCKER H, et al. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional Varus[J]. Clin Orthop Relat Res, 2012, 470(1): 45-53. |
| [8] |
VICTOR J, URLUS M, BELLEMANS J, et al. Femoral intramedullary instrumentation in total knee arthroplasty: the role of pre-operative X-ray analysis[J]. Knee, 1994, 1(2): 123-125. |
| [9] |
王本超, 陈森, 方洪松, 等. 股骨畸形对TKA术后下肢力线及膝关节线的影响[J]. 中国骨与关节损伤杂志, 2018, 33(12): 1247-1250. WANG B C, CHEN S, FANG H S, et al. Influence of femur deformity on lower limb force line and joint line after total knee arthroplasty[J]. Chin J Bone Joint Injury, 2018, 33(12): 1247-1250. |
| [10] |
叶一林, 柴卫兵, 卢宏章, 等. 伴有关节外畸形的膝骨关节炎行全膝关节置换术的治疗体会[J]. 中国骨与关节外科, 2014, 7(5): 399-403. YE Y L, CHAI W B, LU H Z, et al. Clinical experience of total knee arthroplasty for osteoarthritis associated with severe extra-articular femoral deformity[J]. Chin J Bone Joint Surg, 2014, 7(5): 399-403. |
| [11] |
SIKORSKI J M. Alignment in total knee replacement[J]. J Bone Joint Surg Br, 2008, 90(9): 1121-1127. |
| [12] |
MORELAND J R, BASSETT L W, HANKER G J. Radiographic analysis of the axial alignment of the lower extremity[J]. J Bone Joint Surg, 1987, 69(5): 745-749. |
| [13] |
COOKE T D, SLED E A, SCUDAMORE R A. Frontal plane knee alignment: a call for standardized measurement[J]. J Rheumatol, 2007, 34(9): 1796-1801. |
| [14] |
HVID I, NIELSEN S. Tolal condylar knee arthroplasty :Prosthetic component positioning and radiolucent lines[J]. Acta Orthop Scand, 1984, 55(2): 160-165. |
| [15] |
HVID I, NIELSEN S. Total condylar knee arthroplasty: Prosthetic component positioning and radiolucent lines[J]. Acta Orthop Scand, 1984, 55(2): 160-165. |
| [16] |
LEE H J, LIM J W, LEE D H, et al. Slight under-correction using individualized intentional varus femoral cutting leads to favorable outcomes in patients with lateral femoral bowing and varus knee[J]. Knee Surg Sports Traumatol Arthrosc, 2020, 28(5): 1579-1586. |
| [17] |
NISHIDA K, MATSUMOTO T, TAKAYAMA K, et al. Remaining mild Varus limb alignment leads to better clinical outcome in total knee arthroplasty for varus osteoarthritis[J]. Knee Surg Sports Traumatol Arthrosc, 2017, 25(11): 3488-3494. |
| [18] |
MULLAJI A B, MARAWAR S V, MITTAL V. A comparison of coronal plane axial femoral relationships in Asian patients with varus osteoarthritic knees and healthy knees[J]. J Arthroplasty, 2009, 24(6): 861-867. |
| [19] |
YAU W P, CHIU K Y, TANG W M, et al. Coronal bowing of the femur and tibia in Chinese: its incidence and effects on total knee arthroplasty planning[J]. J Orthop Surg (Hong Kong), 2007, 15(1): 32-36. |
| [20] |
WERNER F W, AYERS D C, MALETSKY L P, et al. The effect of valgus/varus malalignment on load distribution in total knee replacements[J]. J Biomech, 2005, 38(2): 349-355. |
| [21] |
SHARKEY P F, HOZACK W J, ROTHMAN R H, et al. Insall Award paper. Why are total knee arthroplasties failing today?[J]. Clin Orthop Relat Res, 2002(404): 7-13. |
| [22] |
GREEN G V, BEREND K R, BEREND M E, et al. The effects of varus tibial alignment on proximal tibial surface strain in total knee arthroplasty: The posteromedial hot spot[J]. J Arthroplasty, 2002, 17(8): 1033-1039. |
| [23] |
BONNER T J, EARDLEY W G P, PATTERSON P, et al. The effect of post-operative mechanical axis alignment on the survival of primary total knee replacements after a follow-up of 15 years[J]. J Bone Joint Surg Br, 2011, 93(9): 1217-1222. |
| [24] |
RITTER M A, DAVIS K E, MEDINGJ B, et al. The effectof alignment and BMl on failure of total knee replacement[J]. J Bonc Joint Surg Am, 2011, 93(17): 1588-1596. |
| [25] |
MORGAN S S, BONSHAHI A, PRADHAN N, et al. The influence of postoperative coronal alignment on revision surgery in total knee arthroplasty[J]. Int Orthop, 2008, 32(5): 639-642. |
| [26] |
VANLOMMEL L, VANLOMMEL J, CLAES s, et al. Slightundercorrection following tolal knee arthroplasty results insuperior clinical outcomes in varus knees[J]. Knec SurgSports 'Traumatol Arthrosc, 2013, 21(10): 2325-2330. |
| [27] |
RITTER M A, DAVIS K E, MEDING J B, et al. The effect of alignment and BMI on failure of total knee replacement[J]. J Bone Joint Surg Am, 2011, 93(17): 1588-1596. |
| [28] |
DELPORT H, LABEY L, INNOCENTI B, et al. Restoration of constitutional alignment in TKA leads to more physiological strains in the collateral ligaments[J]. Knee Surg Sports Traumatol Arthrosc, 2015, 23(8): 2159-2169. |
| [29] |
VANLOMMEL L, VANLOMMEL J, CLAES S, et al. Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees[J]. Knee Surg Sports Traumatol Arthrosc, 2013, 21(10): 2325-2330. |
| [30] |
SCHIFFNER E, WILD M, REGENBRECHT B, et al. Neutral or natural? functional impact of the coronal alignment in total knee arthroplasty[J]. J Knee Surg, 2019, 32(8): 820-824. |
| [31] |
MATZIOLIS G, ADAM J, PERKA C. Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement[J]. Arch Orthop Trauma Surg, 2010, 130(12): 1487-1491. |
| [32] |
PARRATTE S, PAGNANO M W, TROUSDALE R T, et al. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements[J]. J Bone Joint Surg Am, 2010, 92(12): 2143-2149. |




