Pierre Robin综合征(Pierre-Robin syndrome, PRS)又称小颌畸形综合征,以新生儿、婴儿时期的小下颌、下颌后缩、舌后坠、腭裂引起的吸气性呼吸困难、喂养困难为特征[1],其发病率1/20 000~1/8 500[2], 严重者因上气道梗阻导致缺氧而引发一系列并发症,如脑损伤、肺水肿、肺心病及发育停滞[3],甚至死亡[4],死亡率为3.6%~21%[5]。故对于严重PRS患儿尽早有效的治疗是挽救其生命及减少严重并发症、提高生存质量的保证。目前对于严重PRS患儿,下颌骨牵引成骨术(mandibular distraction osteogenesis, MDO)是被广泛认可的有效治疗方法。牵引成骨术完善的术前设计是保证治疗效果的关键,其中最重要的是牵引方向的确定[6-7]。牵引方向由截骨线及牵引器安放的位置决定,故术前精准设计截骨线及延长器安放位置是决定手术效果的关键。本研究对2016-2017年在我院治疗的10例严重PRS患儿,术前利用计算机设计截骨线及模拟延长过程+3D打印头模实体验证截骨、预弯延长器、安放延长器、牵引过程,两者吻合后,3D打印个体化截骨及牵引器安放模块,用于术中指导截骨及安放延长器,该方法取得稳定的治疗效果,现报告如下。
1 资料与方法 1.1 临床资料选取重庆医科大学附属儿童医院烧伤整形科2016-2017年诊治的PRS ColeⅢ级[8]患儿10例,其中男性5例,女性5例。患儿均为出生即刻诊断为PRS,生后因严重上呼吸道梗阻在出生医院立即气管插管后转来我院。入我院年龄1.5~4 d,因在我院新生儿科保守治疗无效、无法拔出气管插管,家属强烈要求手术治疗而转入我科,我科对以上患儿进行双侧MDO治疗。手术年龄8~78(37.5±16.6)d。术前CT示下颌骨后缩,舌根后坠, 舌根、气管插管(内径3~3.5 mm)、咽后壁三者无缝紧贴,舌骨大角至第1颈椎前缘距离/腭板后缘至第1颈椎前缘距离 < 1。
1.2 方法所有患儿术前进行面颌三维螺旋CT(美国GE公司生产的LightSpeed VCT)薄层(0.625 mm)扫描+三维重建,计算机上利用mimics软件进行截骨线设计、延长器安放、模拟牵引至轻度的Ⅲ类错颌畸形[9](图 1),并3D打印头模。在头模上复制计算机软件模拟的截骨、牵引器安放、牵引过程(图 2A、B),进一步验证计算机模拟的正确性后,3D打印个体化截骨及牵引器安放模块(图 2C),并预弯延长器(图 2D),用于术中指导手术。
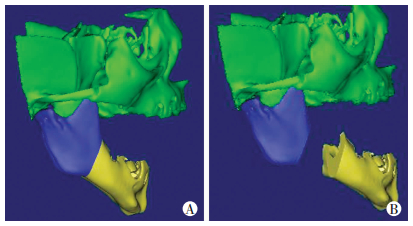
|
| A:计算机设计截骨线;B:计算机模拟截骨及延长 图 1 计算机三维重建模型 |
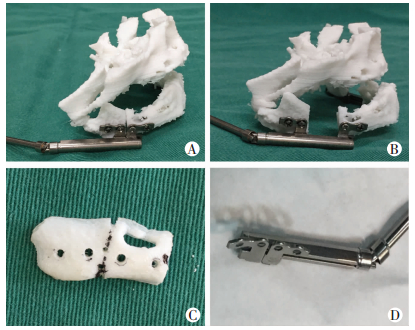
|
| A: 3D头模截骨及延长器安置; B: 3D头模模拟延长; C: 3D打印个体化截骨模块; D:个体化预弯延长器 图 2 3D模型大体观察 |
手术在气管插管全麻下进行,于下颌角及下颌体下缘一横指处做与下颌体平行的长2~2.5 cm的横行切口,切开皮肤、分离皮下、颈阔肌、部分咬肌,暴露下颌角及部分下颌体,切开骨膜,剥离骨膜,将术前设计的个体化模板放入该区,标记截骨线、钛钉固定的位置及下牙槽神经血管束的位置(图 3A)。沿截骨线用超声骨刀全层截开下颌体牙槽嵴顶及下颌下缘骨质,牙槽神经血管束区域仅截开颊侧骨皮质。以薄骨凿凿开截骨线舌侧残余骨皮质连接,充分离断下颌骨体。安放预弯的下颌骨牵引器(浙江宁波磁北公司生产),并按标志进行钛钉固定(图 3B)。记录手术持续时间及出血情况,术后5 d的间歇期后进行常规的牵引成骨治疗,速度为1.2 mm/d,分2次完成。延长至轻度的Ⅲ类错颌畸形后停止延长。记录延长天数及延长距离;延长结束后摄下颌骨CT,测量延长距离、舌根到咽后壁距离,计算舌骨大角至第1颈椎前缘距离/腭板后缘至第1颈椎前缘距离比值;记录拔出气管插管时间、拔管后氧饱和度值、经口喂养情况。做PSG测量AHI。延长结束3个月截骨区域骨愈合后二次手术拆除牵引器。

|
| A:术中截骨模块指导截骨; B:术中延长器安置 图 3 术中截骨及延长器安置 |
2 结果
10例患儿均顺利完成下颌骨牵引成骨治疗。第1次手术时间1.5~2(1.72±0.15)h;出血量10~20(16±3)mL。术后均于第6天开始延长,每日延长2次,每次0.6 mm,延长天数为8~12(9.40±1.08)d。延长结束后摄下颌骨CT,测量延长距离,10例20侧延长距离为9.6~14.4(11.11±1.18)mm(其中5例两侧延长距离出现少许差异,为0.2~1.2 mm,考虑为延长器回缩所致);舌根到咽后壁距离6~8.8(7.17±0.70)mm;术后舌骨大角至第1颈椎前缘距离/腭板后缘至第1颈椎前缘距离≥1。10例患儿延长5~8(6.10± 0.74)d后顺利拔出气管插管,改为面罩给氧,氧饱和度为94%~100%;1~4 d后停止用氧,自然呼吸下氧饱和度为93%~100%。拔管后经口喂养,7 d后8例患儿能每日经口进食奶240~480(374.0±65.2)mL,2例不能经口进食仍需要鼻饲喂养。术后多导睡眠图PSG示呼吸暂停低通气指数AHI 1~3(1.5±0.6)次。面部下1/3明显延长,下颌骨畸形得到显著改善(图 4)。
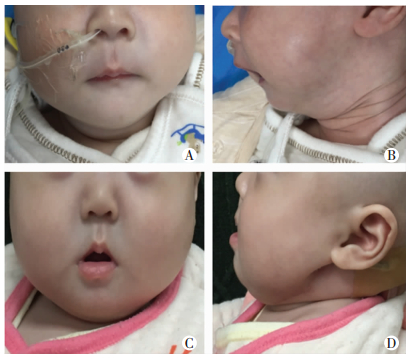
|
| A:术前正位; B:术前侧位; C:术后正位; D:术后侧位 图 4 PRS患儿术前、术后面部情况比较 |
牵引结束后经过3个月的稳定期骨愈合后二期手术拆除牵引器,所有患者的牵引成骨区成骨良好,均未出现成骨不良、牵引故障等严重并发症。拆除牵引器后随访6~12个月,10例患儿均呼吸正常,经口进食可,体质量增加正常,CT示下颌骨后缩矫正满意(图 5)。

|
| A:术前CT正位; B:术前CT侧位; C:术后CT正位; D:术后CT侧位 图 5 PRS患儿术前和术后CT表现 |
3 讨论
MDO是一种公认的治疗严重PRS的有效方法,通过延长下颌骨,而非骨移植,来治疗下颌骨后缩,并增加咽部气道体积、改善呼吸,使大多数患有严重PRS的新生儿和婴儿成功避免了气管切开术[10]。MDO被认为是近年来治疗PRS婴幼儿安全可行的治疗方法[11],并被认为是治疗严重气道阻塞的PRS患者的常规治疗方法[12], 尤其对于保守治疗无效、不宜行唇舌粘连术及气管切开术或效果不满意的这部分患儿,MDO更是一个常规、有效的替代治疗方法[13]。研究发现MDO还能降低腭裂宽度,延长软腭,将U型转变为一个更有利的V型裂口,有利于后期腭裂修补术及术后语音改善[14]。
传统的MDO术前设计是通过影像学资料与临床检查的结果来定位截骨线、牵引器安放的位置及牵引方向,精确度较差,也无法预测牵引结束的时间及颌骨形态[15]。手术过程中两侧截骨线可能无法达到完全精准对称,且受手术切口及周围组织影响,不能暴露大段下颌骨,故牵引器的弧度调整及安放也无法精确。手术操作过程中需反复调整延长器弧度,增加术中操作时间,增加出血量,且仍不能达到最佳服帖效果,术后两侧延长不对称较为常见,且术中不能准确预见下齿槽神经血管走形,术中较易损伤下齿槽神经血管;术后由于固定位置不稳定性,也较易发生钛钉脱落、延长障碍、不对称等并发症。随着计算机软件在医学领域的广泛、深入应用,牵引成骨术的外科手术过程逐渐建立在计算机模拟的基础上,从而使治疗的个性化得以实现[16]。随着3D打印技术在临床的逐渐广泛应用,使得颌面部术前设计及手术模拟变得更加直观、立体[17-18]。
为提高手术精准性,我科术前利用计算机软件设计截骨及模拟延长过程,并3D打印颌部立体准确外观验证该截骨线设计、延长器安放与延长过程,两者吻合后打印个体化截骨及延长器安放模块,并预弯延长器,用于术中指导截骨及延长器安放。该方法可有效减少术中直视范围、缩短手术切口,减少组织剥离损伤,截骨及安放延长器更精准、快捷,减少血管神经损伤。我科采用该方法治疗严重PRS婴儿10例,取得良好效果,手术时间短、术中出血少,较传统MDO手术时间缩短1/4~1/3,出血量减少1/4,10例呼吸均得到明显改善,平均延长6.1 d后均能拔气管插管,自然呼吸下氧饱和度维持93%以上,进食80%得到明显改善。多导睡眠图PSG示AHI(1.5±0.6)次。术后无面神经损伤及延长器脱落、两侧面部不对称等并发症表现,较传统MDO手术,大大减少了并发症的发生。3个月后所有患儿牵引区均未出现骨不连,成骨良好。面部下1/3明显延长,下颌骨后缩得到显著改善,顺利取出延长器。术后随访6~12个月10例患儿均呼吸正常,经口进食可,体质量增加正常,CT示下颌骨后缩矫正满意,家长对治疗效果非常满意。故我们认为术前计算机辅助+3D打印模拟截骨、牵引,并制作个体化截骨及延长器安放模块、个体化预弯延长器不仅能提高严重PRS婴儿MDO中操作的精准性,缩短手术时间,减少出血,并能避免损伤周围重要解剖结构,是严重PRS婴儿MDO的精准操作方法。
| [1] | GANGOPADHYAY N, MENDONCA D A, WOOA S. Pierre robin sequence[J]. Semin Plast Surg, 2012, 26(2): 76–82. DOI:10.1055/s-0032-1320065 |
| [2] | BREUGEM C C, MINK VAN DER MOLEN A B. What is 'Pierre Robin sequence'[J]. J Plast Reconstr Aesthet Surg, 2009, 62(12): 1555–1558. DOI:10.1016/j.bjps.2008.06.050 |
| [3] | JAKOBSEN L P, KNUDSEN M A, LESPINASSE J, et al. The genetic basis of the Pierre Robin Sequence[J]. Cleft Palate Craniofac J, 2006, 43(2): 155–159. DOI:10.1597/05-008.1 |
| [4] | CÔTÉ A, FANOUS A, ALMAJED A, et al. Pierre Robin sequence: review of diagnostic and treatment challenges[J]. Int J Pediatr Otorhinolaryngol, 2015, 79(4): 451–464. DOI:10.1016/j.ijporl.2015.01.035 |
| [5] | GÖZV A, GENÜ B, PALABIYIK M, et al. Airway management in neonates with Pierre Robin sequence[J]. Turk J Pediatr, 2010, 52(2): 167–172. |
| [6] | VENDITTELLI B L, DEC W, WARREN S M, et al. The importance of vector selection in preoperative planning of bilateral mandibular distraction[J]. Plast Reconstr Surg, 2008, 122(4): 1144–1153. DOI:10.1097/PRS.0b013e318185d596 |
| [7] | GATENO J, ALLEN M E, TEICHGRAEBER J F, et al. An in vitro study of the accuracy of a new protocol for planning distraction osteogenesis of the mandible[J]. J Oral Maxillofac Surg, 2000, 58(9): 985–990. DOI:10.1053/joms.2000.8740 |
| [8] | COLE A, LYNCH P, SLATOR R. A new grading of Pierre Robin sequence[J]. Cleft Palate Craniofac J, 2008, 45(6): 603–606. DOI:10.1597/07-129.1 |
| [9] |
赵竟伊, 靳小雷. 下颌骨牵引成骨技术在婴幼儿Pierre Robin序列征治疗中的应用进展[J].
中华整形外科杂志, 2014, 30(2): 157–160.
ZHAO J Y, JIN X L. Application progress of mandibular distraction osteogenesis in the treatment of infants with Pierre Robin syndrome[J]. Chin J Plastic Surg, 2014, 30(2): 157–160. DOI:10.3760/cma.j.issn.1009-4598.2013.02.25 |
| [10] | CHING J A, DAGGETT J D, ALVAREZ S A, et al. A simple mandibular distraction protocol to avoid tracheostomy in patients with Pierre Robin sequence[J]. Cleft Palate Craniofac J, 2017, 54(2): 210–215. DOI:10.1597/14-211 |
| [11] | RACHMIEL A, EMODI O, RACHMIEL D, et al. Internal mandibular distraction to relieve airway obstruction in children with severe micrognathia[J]. Int J Oral Maxillofac Surg, 2014, 43(10): 1176–1181. DOI:10.1016/j.ijom.2014.06.013 |
| [12] | SAHOO N K, ROY I D, DALAL S, et al. Distraction osteogenesis for management of severe OSA in Pierre Robin sequence: an approach to elude tracheostomy in infants[J]. J Maxillofac Oral Surg, 2016, 15(4): 501–505. DOI:10.1007/s12663-016-0888-4 |
| [13] | MACKAY D R. Controversies in the diagnosis and management of the Robin sequence[J]. J Craniofac Surg, 2011, 22(2): 415–420. DOI:10.1097/SCS.0b013e3182074799 |
| [14] | COLLARES M V, DUARTE D W, SOBRAL D S, et al. Neonatal mandibular distraction osteogenesis reduces cleft palate width and lengthens soft palate, influencing palatoplasty in patients with Pierre Robin sequence[J]. J Craniofac Surg, 2016, 27(5): 1267–1272. DOI:10.1097/SCS.0000000000002752 |
| [15] |
李阳, 伊彪, 王兴, 等. 三维头模设计及个体化模板引导技术在OSAHS患者下颌骨牵引成骨术中的应用[J].
中华口腔正畸学杂志, 2014, 21(2): 95–99.
LI Y, YI B, WANG X, et al. Application of 3D head mold planning and individualized templates in mandibular distraction[J]. Chin J Orthodont, 2014, 21(2): 95–99. DOI:10.3760/cma.j.issn.1674-5760.2014.02.009 |
| [16] | SŁOWIŃSKI J J, CZARNECKA A. Numerical modeling of the traction process in the treatment for Pierre-Robin sequence[J]. Int J Pediatr Otorhinolaryngol, 2016, 89: 86–91. DOI:10.1016/j.ijporl.2016.07.030 |
| [17] | METZGER M C, HOHLWEG-MAJERT B, SCHWARZ U, et al. Manufacturing splints for orthognathic surgery using a three-dimensional printer[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2008, 105(2): e1–e7. DOI:10.1016/j.tripleo.2007.07.040 |
| [18] | COHEN A, LAVIV A, BERMAN P, et al. Mandibular reconstruction using stereolithographic 3-dimensional printing modeling technology[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2009, 108(5): 661–666. DOI:10.1016/j.tripleo.2009.05.023 |



